
Eye is a complex organ which is the window to the world outside. It can be affected by many diseases. To know about some common diseases of the eye read on.
Wondering when you or your family members should have their eyes examined by an Eye Specialist?
Read below: If you have any of these risk factors for eye problems, you will need to see your eye specialist more often than recommended below:
Since it is possible for your child to have a serious vision problem without being aware of it, your child should have his or her eyes screened at age 3 and 5 by an eye care professional to screen for eye conditions such as:
If there is a family history of vision problems or if your child appears to have any of the above conditions show to an Eye Specialist immediately
Age 5 to 39Most young people have healthy eyes, but still need to take care of their vision by wearing protective eyewear when working in dangerous areas, playing sports, doing woodwork or yard work, working with chemicals or taking part in other activities that could cause eye injury. Have a complete eye exam at least twice between the ages of 20 and 29 and at least 2 yearly between the ages of 30 and 39. You should also be aware of symptoms that could indicate a problem. See an Eye specialist promptly if you experience any eye problems such as:
Even the young adult and middle age groups can be affected by eye problems, so preventive measures should be taken to protect eyes from injury and detect disease early, especially because this is usually the age when problems like near vision difficulty ,Glaucoma , etc. sets in. Schedule a comprehensive eye evaluation with your Eye Specialist preferably every year.
Over Age 65Seniors 65 and older should have comprehensive eye evaluations by their Eye Specialist compulsorily every year to test for cataracts, glaucoma, age-related macular degeneration and other eye conditions
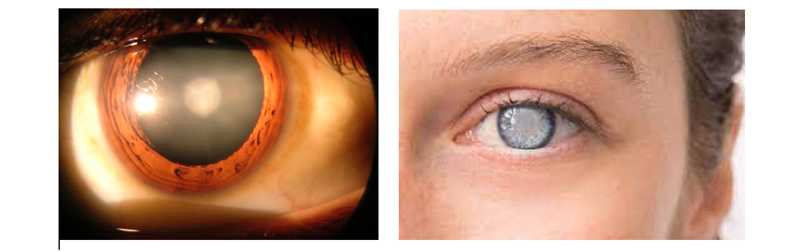
Cataract is a clouding of the eyes naturally clear lens. The lens focuses light rays on the retina , the layer of light-sensing cells lining the back of the eye , to produce a sharp image of what we see. When the lens becomes cloudy, light rays cannot pass through it easily, and vision is blurred.
What causes cataracts?
Cataract development is a normal process of aging, but cataracts also develop from eye injuries, certain diseases, or medications. Your genes may also play a role in cataract development.
How can a cataract be treated?
A cataract may not need to be treated if your vision is only slightly blurry. Simply changing your eyeglass prescription may help to improve your vision for a while. There are no medications, eye drops, exercises or glasses that will cause cataracts to disappear once they have formed. Surgery is the only way to remove a cataract. When you are no longer able to see well enough to do the things you like to do, or when the doctor advises, cataract surgery should be considered.
Cataract Surgery
In cataract surgery, the cloudy lens is removed from the eye through a surgical incision. The procedure is called phacoemulsification or microincision cataract surgery (MICS) In most cases, the natural lens is replaced with a permanent intraocular lens (IOL) implant. At Tirupati Eye Centre, the Stellaris Bausch & Lomb platform is used, which is one of the best platforms worldwide for microincision cataract surgery as it can remove cataract through the SMALLEST POSSIBLE INCISION of 1.4 mm.

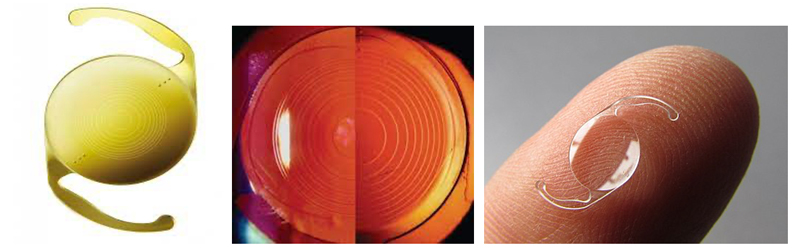
What are the different types of lenses?
Intraocular lenses can be of various types:
All these lenses have their pros and cons and the decision about which lens to implant has to be taken by the patient in consultation with the doctor.
What can I expect if I decide to have cataract surgery?
Before Surgery
To determine if your cataract should be removed, your doctor will perform a thorough eye examination. It is advisable to not wait for the cataract to mature i.e. become total as was previously believed because once mature, the cataract can raise the pressure of the eye resulting in lens induced glaucoma which can cause a permanent damage to the optic nerve. Before surgery, your eye will be measured to determine the proper power of the intraocular lens that will be placed in your eye.
The Day of Surgery
Surgery is usually done on an outpatient basis (day care surgery) in the hospital. The hospital stay is around 4-5 hours, And the procedure itself takes around 8-10 minutes to be completed, the incision made in this procedure is very small (1.8 mm). It is a painless procedure which is done in majority of cases under topical anaesthesia (eye drops are used to numb the eye). During cataract surgery, tiny instruments are used to break apart and remove the cloudy lens from the eye. After removing the cataractous lens, an artificial lens called intraocular lens (IOL) is implanted inside the eye.
Following Surgery
You will need to:
The lens capsule (the part of the eye that holds the lens in place) sometimes becomes cloudy months or years after the original cataract operation in 10-20 % of cases. If the cloudy capsule blurs your vision, your ophthalmologist can perform a second procedure using a laser. No surgery is usually required. During the second procedure, called a posterior capsulotomy, a laser is used to make an opening in the cloudy lens capsule, restoring normal vision.
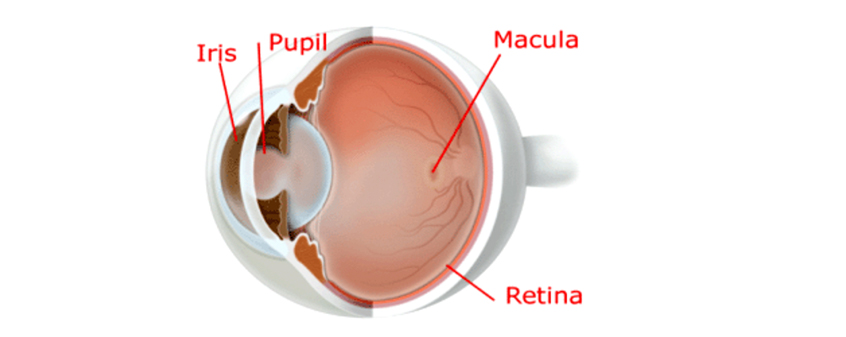
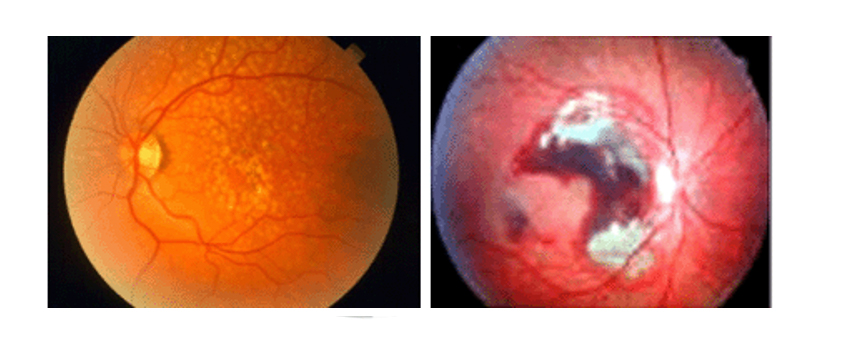
Diabetes is a disease which is very common nowadays and it can damage the retina and this is called diabetic retinopathy. The retinal blood vessels become weak and hence bleed leak. Or they can close, stopping blood from passing through. Sometimes abnormal new fragile blood vessels can also grow on the retina in advanced stages. All of these changes can cause a fall in vision.
Diabetic retinopathy has 2 main stages
NPDR (non-proliferative diabetic retinopathy)
This is an early stage which is seen in many diabetics after 5 years of diabetes.
In this stage, blood vessels leak, making the retina swell. When the macula (main part of eye responsible for 90% vision) swells, it is called macular edema. Macular edema is the commonest cause of loss of vision due to diabetes.
In NPDR, blood vessels in the retina can become very thin decreasing the blood supply to the retina resulting in macular ischemia. In some cases, due to leakage small yellow spots are seen called exudates which also block vision.
PDR (proliferative diabetic retinopathy)
PDR is an advanced stage of diabetic eye disease in which retina starts developing new blood vessels, which is called neovascularization. These new vessels are fragile and often bleed into the retina and the vitreous cavity. This can result in “floaters” or sudden loss of vision. Sometimes there can be a pull on the retina which is called traction and this can result in retina to detach from its position, called retinal detachment.
PDR is a serious condition and can result in blindness.
What are the symptoms of diabetic retinopathy?
In the early and middle stages diabetic retinopathy has no symptoms. With time the following symptoms can develop:
Diagnosis of diabetic retinopathy
Treatment of diabetic retinopathy
Lasers
Lasers might be needed in some cases to help seal leaking blood vessels as well as to reduce the swelling of the retina. This can also help shrink blood vessels. Sometimes more than one treatment is needed as a combination.
Vitrectomy surgery
In advanced cases of proliferative diabetic retinopathy, the doctor may recommend surgery called vitrectomy. In this surgery, the vitreous gel is removed and blood from leaking vessels in the back of the eye also removed. This allows the vision to improve.
Recommended schedule for retina check-up for diabetics
Type 1 DM: 1st Retinal exam 3-5 years after diagnosis
Type 2 DM: 1st Retinal exam at the time of diagnosis
Pregnancy (with type 1 or type 2): 1st Retinal exam soon after conception and early in the 1st trimester of pregnancy
An eye examination is not required if patients without DM newly develop gestational diabetes during pregnancy.
Macular degeneration is a deterioration or breakdown of the macula. The macula is a small area in the retina at the back of the eye that allows to see fine details clearly. When the macula does not function correctly, central vision can be affected by blurriness, dark areas or distortion. Macular degeneration affects your ability to see near and far and can make some activities — like threading a needle or reading — difficult or impossible.
Macular degeneration alone does not result in total blindness. Even in more advanced cases, people continue to have some useful vision and are often able to take care of themselves. In many cases, macular degenerations impact on your vision can be minimal.
What causes macular degeneration?
Many older people develop macular degeneration as part of the body’s natural aging process. There are different kinds of macular problems, but the most common is age-related macular degeneration (AMD). Exactly why it develops is not known, and no treatment has been uniformly effective.
The two most common types of AMD are "dry" (atrophic) and "wet" (exudative):
"Dry" macular degeneration (atrophic)- Most people have the "dry" form of AMD. It is caused by aging and thinning of the tissues of the macula. Vision loss is usually gradual.
"Wet" macular degeneration (exudative)- The "wet" form of macular degeneration accounts for about 10 percent of all AMD cases. It results when abnormal blood vessels form underneath the retina grow either behind or into the retina. These new blood vessels leak fluid or blood and blur central vision. Vision loss may be rapid and severe.
Deposits under the retina called drusen are a common feature of macular degeneration. Drusen alone usually do not cause vision loss, but when they increase in size or number, this generally indicates an increased risk of developing advanced AMD. People at risk for developing advanced wet AMD in the eye have significant drusen, prominent dry AMD, or abnormal blood vessels under the macula in one eye ("wet" form).
Dry and wet AMD
What are the symptoms of macular degeneration?
Macular degeneration can cause different symptoms in different people. The condition may be hardly noticeable in its early stages. Sometimes only one eye loses vision while the other eye continues to see well for many years. But when both eyes are affected, the loss of central vision may be noticed more quickly.
Following are some common ways vision loss is detected:
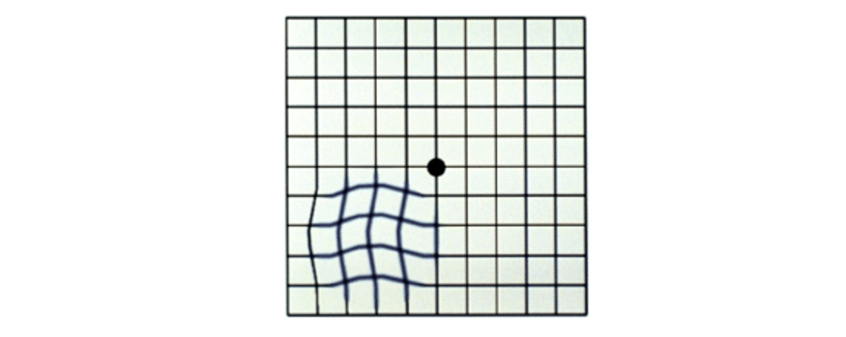
Amsler grid with wavy lines
How is macular degeneration diagnosed?
Many people do not realize that they have a macular problem until blurred vision becomes obvious. The doctor can detect early stages of AMD during a medical eye examination that includes the following:
How is macular degeneration treated?
Nutritional Supplements
Though the exact causes of macular degeneration are not fully understood, antioxidant vitamins and zinc may reduce the impact of AMD in some people.
A large scientific study found that people at risk for developing advanced stages of AMD lowered their risk by about 25 percent when treated with a high-dose combination of vitamin C, vitamin E, beta carotene and zinc. It is very important to remember that vitamin supplements are not a cure for AMD, nor will they restore vision that you may have already lost from the disease. However, specific amounts of these supplements do play a key role in helping some people at high risk for advanced AMD to maintain their vision. You should speak with your ophthalmologist to determine if you are at risk for developing advanced AMD, and to learn if supplements are recommended for you.
Anti-VEGF Treatments
Anti VEGF injections is a modality which is giving excellent result in management of wet AMD. It targets a specific chemical in your body that is critical in causing abnormal blood vessels to grow under the retina. This chemical is called vascular endothelial growth factor (VEGF).
Anti-VEGF drugs block the trouble-causing VEGF, reducing the growth of abnormal blood vessels and slowing their leakage. This is probably the only treatment for wet AMD which actually improves the vision in some cases.
These procedures may preserve more sight overall, though they are not cures that restore vision to normal. Despite advanced medical treatment, many people with macular degeneration may still experience some vision loss.
Injections need to be repeated at intervals, as per advice of the doctor.
Testing Your Vision with the Amsler Grid
You can check your vision daily by using an Amsler grid like the one pictured here. You may find changes in your vision that you would notnotice otherwise. Putting the grid on the front of your refrigerator is a good way to remember to look at it each day.
Amsler Grid
To use the grid:
You may sometimes see small specks or clouds moving in your field of vision. They are called floaters. You can often see them when looking at a plain background, like a blank wall or blue sky.
Floaters are actually tiny clumps of gel or cells inside the vitreous , the clear jelly-like fluid that fills the inside of your eye.
Although the floaters appear to be in front of the eye, they are actually floating in the vitreous fluid inside the eye.
While these objects look like they are in front of your eye, they are actually floating inside. What you see are the shadows they cast on the retina , the nerve layer at the back of the eye that senses light and allows you to see.
Floaters can have different shapes: little dots, circles, lines, clouds or cobwebs.
What causes floaters?When people reach middle age, the vitreous gel may start to thicken or shrink, forming clumps or strands inside the eye. The vitreous gel pulls away from the back wall of the eye, causing a posterior vitreous detachment . It is a common cause of floaters. Other causes could be trauma, inflammation and myopia.
Posterior vitreous detachment is more common for people who:
The appearance of floaters may be alarming, especially if they develop suddenly. You should also see an ophthalmologist immediately if you suddenly develop new floaters.
Are floaters ever serious?The retina can tear if the shrinking vitreous gel pulls away from the wall of the eye. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters.
A torn retina is always a serious problem, since it can lead to a retinal detachment. You should see your ophthalmologist as soon as possible if:
If you notice other symptoms, like the loss of side vision like a curtain or shadow, you should see your ophthalmologist immediately as this suggests a retinal detachment. This is a serious condition which causes sudden loss of vision which is at times not fully retrievable even with surgical Management.
Retinal tears can result in a retinal detachment Retinal detachment in the upper part of retina
Laser barrage around the tear can prevent a retinal detachment
What can be done about floaters?Because you need to know if your retina is torn, get yourself examined by your ophthalmologist if a new floater appears suddenly.
Floaters can get in the way of clear vision, which may be quite annoying, especially if you are trying to read. You can try moving your eyes, looking up and then down to move the floaters out of the way.
While some floaters may remain in your vision, many of them will fade over time and become less bothersome. Even if you have had some floaters for years, you should have an eye examination immediately if you notice new ones.
What causes flashes of lights?When the vitreous gel rubs or pulls on the retina, you may see what look like flashing lights or lightning streaks. You may have experienced this same sensation if you have ever been hit in the eye and seen "stars."
When the vitreous rubs or pulls on the retina, it creates a sensation of flashing lights.
The flashes of light can appear off and on for several weeks or months. As we grow older, it is more common to experience flashes. If you notice the sudden appearance of light flashes, you should visit your ophthalmologist immediately to see if the retina has been torn.
How are your eyes examined?When an ophthalmologist examines your eyes, your pupils will be dilated with eye drops. During this painless examination, your ophthalmologist will carefully observe your retina and vitreous.
Floaters and flashes of light become more common as we grow older. While not all floaters and flashes are serious, you should always have an eye examination by an ophthalmologist to make sure there has been no damage to your retina.
Glaucoma is a disease of the optic nerve — the part of the eye that carries the images we see to the brain. The optic nerve is made up of many nerve fibers, like an electric cable containing numerous wires. When damage to the optic nerve fibers occurs, blind spots develop. These blind spots usually go undetected until the optic nerve is significantly damaged. When the entire nerve gets destroyed the person would go blind.
Early detection and treatment by your ophthalmologist are the keys to preventing optic nerve damage and blindness from glaucoma. Loss of sight from glaucoma can often be prevented with early treatment.
What causes glaucoma?Clear liquid called aqueous humor circulates inside the front portion of the eye. To maintain a healthy level of pressure within the eye, a small amount of this fluid is produced constantly while an equal amount flows out of the eye through a microscopic drainage system. (This liquid is not part of the tears on the outer surface of the eye.)
Because the eye is a closed structure, if the drainage area for the aqueous humor — called the drainage angle — is blocked, the excess fluid cannot flow out of the eye. Fluid pressure within the eye increases, pushing against the optic nerve and causing damage.
Clear liquid called aqueous humor is constantly being produced within the eye (left). If the drainage angle of the eye is blocked, fluid cannot flow out of the eye (right).
What are the different types of glaucoma? Chronic open-angle glaucoma:This is the most common form of glaucoma. The risk of developing chronic open-angle glaucoma increases with age. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, which can damage the optic nerve. In some patients, the optic nerve is sensitive even to normal eye pressure and is at risk for damage. Treatment is necessary to prevent further vision loss.
Typically, open-angle glaucoma may have no symptoms or vague symptoms like headache or frequent change of power of glasses, etc in its early stages and vision remains normal. As the optic nerve becomes more damaged, blank spots begin to appear in the field of vision. You typically wont notice these blank spots in your day-to-day activities until the optic nerve is significantly damaged and these spots become large. When the entire nerve gets destroyed the person would go blind.
Closed-angle glaucoma:Some eyes are formed with the iris (the colored part of the eye) too close to the drainage angle. In these eyes, which are often small and farsighted, the iris can be pushed into the drainage angle and block it completely. Since the fluid cannot exit the eye, pressure inside the eye builds rapidly and causes an acute closed-angle attack.
Symptoms may include:
This is a true eye emergency. If you have any of these symptoms, go to your ophthalmologist immediately. Unless this type of glaucoma is treated quickly, blindness can result.
Though some patients may show some less severe symptoms suggestive of this condition most with closed-angle glaucoma, unfortunately, develop it slowly without any symptoms prior to an attack.
Who is at risk for glaucoma?Your ophthalmologist considers many kinds of information to determine your risk for developing the disease.
The most important risk factors include:
Your ophthalmologist will weigh all of these factors before deciding whether you need treatment for glaucoma, or whether you should be monitored closely as a glaucoma suspect. This means your risk of developing glaucoma is higher than normal, and you need to have regular examinations to detect the early signs of damage to the optic nerve.
Glaucomatous optic nerve - large central white cup signifies damaged peripheral nerve fibres
How is glaucoma detected?Regular eye examinations by your ophthalmologist are the best way to detect glaucoma. A glaucoma screening that checks only the pressure of the eye is not sufficient to determine if you have glaucoma. The only sure way to detect glaucoma is to have a complete eye examination.
During your glaucoma evaluation, your ophthalmologist will:
Automated Perimeter-an automated instrument used to test peripheral field of vision
Decreased field or vision in glaucoma

Field chart of perimetry showing defects
Photography of the optic nerve or other computerized imaging may be recommended. Some of these tests may not be necessary for everyone. These tests may need to be repeated on a regular basis to monitor any changes in your condition.
How is glaucoma treated?As a rule, damage caused by glaucoma cannot be reversed. Eye drops, laser and surgery in the operating room are used to help prevent further damage. In some cases, oral medications also may be prescribed. With any type of glaucoma, periodic examinations are very important to prevent vision loss. Because glaucoma can progress without your knowledge, adjustments to your treatment may be necessary from time to time.
MedicationsGlaucoma is usually controlled with eye drops taken daily. These medications lower eye pressure.
Never change or stop taking your medications without consulting your ophthalmologist. If you are about to run out of your medication, ask your ophthalmologist if you should continue with the same. Glaucoma medications can preserve your vision, but they also may produce side effects. You should notify your ophthalmologist if you think you may be experiencing side effects.
Some eye drops may rarely cause:
All medications can have side effects or can interact with other medications. Therefore, it is important that you make a list of the medications you regularly take and share this list with each doctor you see.
Laser SurgeryLaser surgery treatments may be recommended for different types of glaucoma. In open-angle glaucoma, the drain itself is treated. The laser is used to modify the drain (trabeculoplasty) to help control eye pressure. In closed-angle glaucoma, the laser creates a hole in the iris (iridotomy) to improve the flow of aqueous fluid to the drain.
Surgery in the Operating RoomWhen surgery in the operating room is needed to treat glaucoma, your ophthalmologist uses fine, microsurgical instruments to create a new drainage channel for the aqueous fluid to leave the eye. Surgery is recommended if your ophthalmologist feels it is necessary to prevent further damage to the optic nerve. Nowadays special valves are also available which when implanted in the eye during surgery are giving good control over the intraocular pressure.
What is your part in treatment?Treatment for glaucoma requires teamwork between you and your doctor. Your ophthalmologist can prescribe treatment for glaucoma, but only you can make sure that you follow your doctors instructions and take your eye drops. Once you are taking medications for glaucoma, your ophthalmologist will want to see you more frequently. Typically, you can expect to visit your ophthalmologist every three to four months. This will vary depending on your treatment needs.
Loss of vision can be preventedRegular medical eye exams may help prevent unnecessary vision loss. Recommended intervals for eye exams are:
Uveitis is a condition in which the middle layer of the eye gets inflamed. This layer is called the uvea. Uveitis can damage important eye tissues and can cause a permanent vision loss.
Types of uveitis
There are 3 types of uveitis based on which part of the uvea is affected.
Sometimes all layers may be involved, and this is called Panuveitis
What are the causes of uveitis?
In approx. 50% cases there is no known cause. However, in the following cases the chances increase:
Symptoms of uveitis
Symptoms can include:
Diagnosis of uveitis
The doctor examines the eye on slit lamp. Since uveitis is often associated with other diseases or conditions, some investigations are advised. These include a physician examination, blood or skin tests, examination of eye fluids, and imaging tests, such as X-rays.
How is uveitis treated?
Uveitis needs to be treated well in time. Generally, it need treatment with steroid eye drops and few other eye drops which dilate the eye. Sometimes medicine may need to be given by injection or as oral tablets. In some cases, opinion has to be taken from a rheumatologist.
 MyoSTOP Myopia Control Centre was launched in August 2023. This is the one of its kind dedicated Myopia Clinic for control of Myopia progression in children
MyoSTOP Myopia Control Centre was launched in August 2023. This is the one of its kind dedicated Myopia Clinic for control of Myopia progression in children
 Tirupati Eye Centre now launches the latest and safest Lasik Laser technology Teneo 2 by Bausch & Lomb with "Bladeless Flapless Touchless" Lasik laser.
Tirupati Eye Centre now launches the latest and safest Lasik Laser technology Teneo 2 by Bausch & Lomb with "Bladeless Flapless Touchless" Lasik laser.
 Project Drishti was inaugurated in August,2023 in which Rotary Club of Noida and Tirupati Eye Centre jointly started free operation of Cataract. In the first session, 100 free operations will be done in 3 months. These operations will be done in those people who are unable to get their operations done due to lack of money.
Project Drishti was inaugurated in August,2023 in which Rotary Club of Noida and Tirupati Eye Centre jointly started free operation of Cataract. In the first session, 100 free operations will be done in 3 months. These operations will be done in those people who are unable to get their operations done due to lack of money.
 Introducing Our Specialized Dry Eye Clinic: We're excited to announce our new clinic in which we do an advanced investigation with an equipment called IDRA which detects the level of abnormality in the tear film and we use the advanced IRPL E-Eye therapy to treat dry eye due to Meibomian gland dysfunction
Introducing Our Specialized Dry Eye Clinic: We're excited to announce our new clinic in which we do an advanced investigation with an equipment called IDRA which detects the level of abnormality in the tear film and we use the advanced IRPL E-Eye therapy to treat dry eye due to Meibomian gland dysfunction
 We are delighted to introduce our cutting-edge Keratoconus Clinic, dedicated to providing expert care and innovative treatments for those dealing with this Keratoconus.
We are delighted to introduce our cutting-edge Keratoconus Clinic, dedicated to providing expert care and innovative treatments for those dealing with this Keratoconus.
 Dr Mohita Sharma elected as Vice President Rotary Club of Noida for philanthropic social work.
Dr Mohita Sharma elected as Vice President Rotary Club of Noida for philanthropic social work.
Shop No. CM FF 25,
AWHO, Gurjinder Vihar, Gr. Noida
Uttar Pradesh (INDIA)
Google Location